Numerous persons who have been infected with SARS-CoV-2 will almost certainly make antibodies in opposition to the virus for most of their lives. So recommend researchers who have discovered extended-lived antibody-making cells in the bone marrow of men and women who have recovered from COVID-191.
The research provides proof that immunity triggered by SARS-CoV-2 infection will be extraordinarily long-lasting. Including to the fantastic information, “the implications are that vaccines will have the very same tough effect”, suggests Menno van Zelm, an immunologist at Monash College in Melbourne, Australia.
Antibodies — proteins that can recognize and assist to inactivate viral particles — are a critical immune defence. Following a new an infection, quick-lived cells known as plasmablasts are an early resource of antibodies.
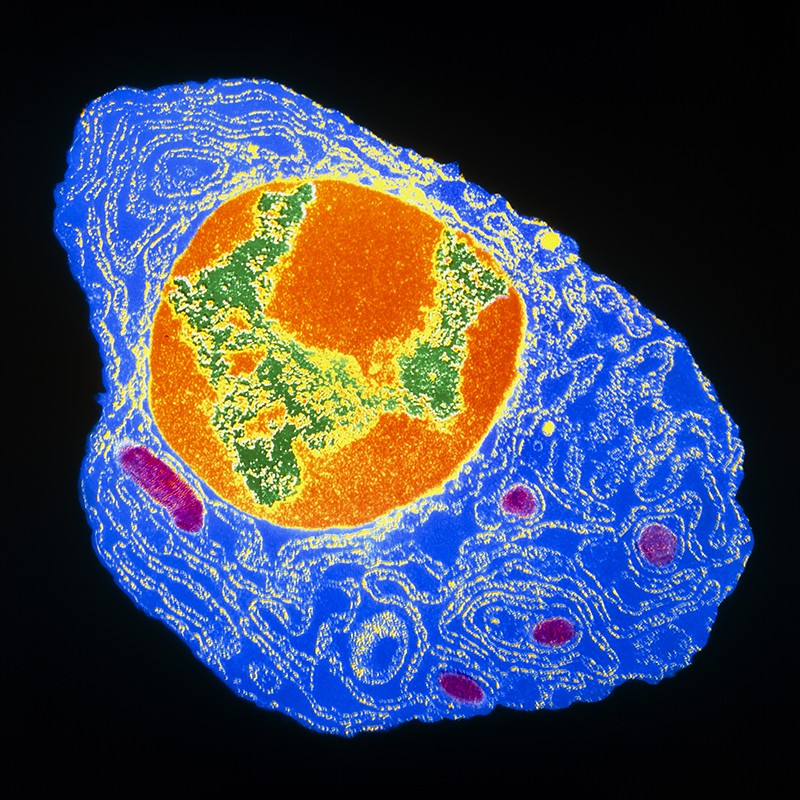
But these cells recede before long immediately after a virus is cleared from the human body, and other, longer-long lasting cells make antibodies: memory B cells patrol the blood for reinfection, while bone marrow plasma cells (BMPCs) hide absent in bones, trickling out antibodies for decades.
“A plasma cell is our lifetime heritage, in conditions of the pathogens we have been exposed to,” states Ali Ellebedy, a B-mobile immunologist at Washington University in St. Louis, Missouri, who led the examine, published in Nature on 24 May perhaps.
Scientists presumed that SARS-CoV-2 an infection would cause the development of BMPCs — almost all viral infections do — but there have been symptoms that critical COVID-19 could possibly disrupt the cells’ development2. Some early COVID-19 immunity studies also stoked problems, when they found that antibody ranges plunged not lengthy soon after recovery3.
Ellebedy’s group tracked antibody generation in 77 persons who had recovered from mostly gentle instances of COVID-19. As anticipated, SARS-CoV-2 antibodies plummeted in the 4 months right after infection. But this drop slowed, and up to 11 months following infection, the researchers could nevertheless detect antibodies that acknowledged the SARS-CoV-2 spike protein.
To recognize the source of the antibodies, Ellebedy’s crew gathered memory B cells and bone marrow from a subset of members. 7 months just after establishing indications, most of these participants even now experienced memory B cells that acknowledged SARS-CoV-2. In 15 of the 18 bone-marrow samples, the experts found extremely-very low but detectable populations of BMPCs whose formation had been activated by the individuals’ coronavirus bacterial infections 7–8 months ahead of. Concentrations of these cells were being stable in all five individuals who gave another bone-marrow sample a number of months later on.
“This is a extremely crucial observation,” specified statements of dwindling SARS-CoV-2 antibodies, states Rafi Ahmed, an immunologist at Emory University in Atlanta, Ga, whose crew co-found the cells in the late 1990s. What’s not distinct is what antibody ranges will look like in the very long term and irrespective of whether they provide any defense, Ahmed provides. “We’re early in the activity. We’re not hunting at 5 several years, 10 yrs immediately after an infection.”
Ellebedy’s team has noticed early signs that Pfizer’s mRNA vaccine need to trigger the generation of the exact cells4. But the persistence of antibody generation, whether elicited by vaccination or by infection, does not assure extended-long lasting immunity to COVID-19. The capability of some rising SARS-CoV-2 variants to blunt the protective consequences of antibodies indicates that extra immunizations could be wanted to restore levels, claims Ellebedy. “My presumption is, we will need to have a booster.”